Please Help Us With the Medicare Plan Mess, State Regulators Ask CMS
What You Need to Know
Many hospitals and physician group practices are giving up on low-paying Medicare Advantage patients.
People much over 65 who want to use Medigap to fill in original Medicare usually face medical underwriting.
State regulators wonder if displaced Medicare Advantage enrollees will qualify for easy Medigap access.
A flood of sick new Medigap enrollees could destabilize the Medigap market.
State insurance regulators say they have no idea what to tell patients panicked by the big Medicare Advantage plan provider network changes coming in 2025.
Plans are supposed to send notices to enrollees about how their provider networks, benefits and other coverage terms will change in 2025 by Sept. 30. State regulators are asking Chiquita Brooks-LaSure, the administrator of the Centers for Medicare and Medicaid Services, for advice about how CMS will handle Medicare Advantage plan upheaval.
Because of the major network changes looming, “beneficiaries are faced with either paying the increased out-of-network costs or rescheduling their necessary medical services with another provider who may not have prompt availability,” officers at the National Association of Insurance Commissioners write in a letter sent Wednesday to Brooks-LaSure.
That means a failure by CMS to answer questions and come up with solutions could hurt some patients’ health, by causing those patients to put off getting medically necessary care, the NAIC officers warn.
The Senior Issues Task Force, an arm of the NAIC, has posted a copy of the letter under the documents tab in its section of the NAIC’s website.
What it means: For financial professionals who have clients enrolled in Medicare Advantage plans, the impact of the 2025 plan changes could be comparable to the effects of the 2007-2009 Great Recession and the COVID-19 pandemic.
If CMS officials, insurers and health care providers do not find a way to reduce the impact of the plan changes, even financial professionals who have nothing to do with selling Medicare Advantage plans or related products and services themselves may finding themselves trying to advise clients who have no idea where else to turn for help.
The NAIC officials point out that state insurance department employees are already getting many difficult questions from consumers affected by the plan changes.
“State departments of insurance across the country are fielding consumer inquiries about the withdrawal of their providers from MA plans,” officials write. “Since states do not regulate these plans, [Department of Insurance] staff are unable to offer recommendations to consumers beyond referring them to CMS or the administrator of their MA plan.”
The changes could also have a bearing on the November general elections, because the plan changes and resulting confusion are hitting as enrollees and their relatives are about to vote.
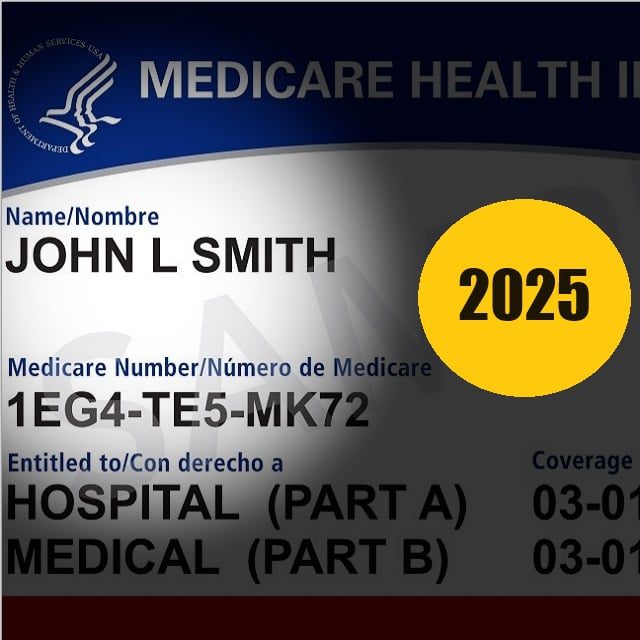
The background: Medicare is a federal program that uses revenue from federal payroll taxes to pay for care for people ages 65 and older, some people with disabilities and some people with severe kidney disease.
The original Medicare program was designed in the 1960s and exposes enrollees to many deductibles, coinsurance bills and copayment costs.
About 34 million of the 67 million enrollees use Medicare Advantage plans, which are regulated at the federal level, to fill coverage gaps in in original Medicare.




