Helping First-Time Medicare Enrollees
What You Need to Know
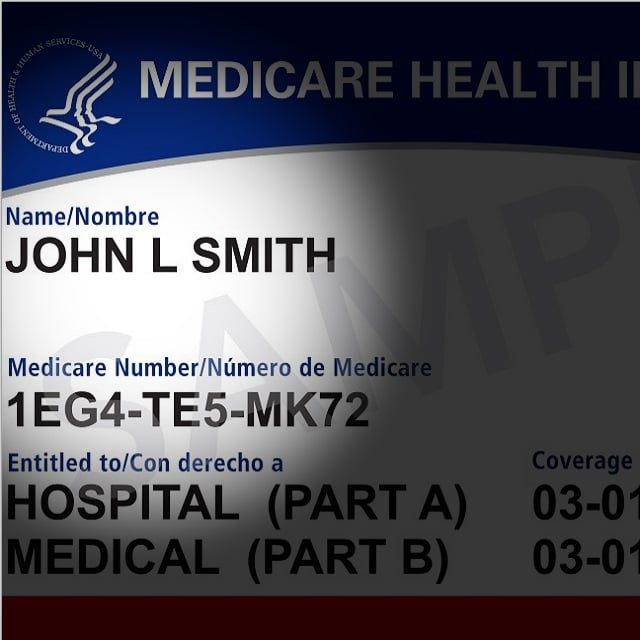
Have eligible clients signed up for Medicare medical coverage?
What about drug benefits?
Do the plans selected cover the doctors, hospitals and prescriptions the clients use?
As the much-publicized annual Medicare enrollment period unfolds, it’s easy to overlook the needs of clients who are becoming eligible for Medicare coverage for the first time.
Missteps during this phase can result in penalties, coverage gaps or increased expenses.
A thorough understanding of the first-time enrollment process is key to helping clients make informed choices.
The Question
What are the most common errors clients make during the Medicare initial enrollment period, or IEP, and how can clients navigate these challenges effectively?
The Answer
The Medicare enrollment process is laden with nuances that, if overlooked, can lead to significant financial and coverage implications.
Here are eight key areas where mistakes are commonly made.
1. Missed Enrollment Deadlines
One of the most critical errors is missing the IEP surrounding one’s 65th birthday.
This oversight can lead to delayed coverage and lifetime penalties.
It’s essential to enroll during this seven-month period, which begins three months before and ends three months after the month of your 65th birthday, unless you qualify for a special enrollment period later.
2. Prescription Drug Plan Oversights
Often, new enrollees neglect to sign up for a Medicare Part D prescription drug plan when opting for Original Medicare.
This omission can result in a late enrollment penalty if they decide to join a Part D plan later.
Since this penalty increases the longer you delay enrollment, it’s advisable to join a Part D plan during your IEP or ensure you have other creditable prescription drug coverage.
3. Special Enrollment Period Confusion
Many people who are still working past 65 or have health insurance through a spouse’s employer miss the opportunity to use the post-employment special enrollment period, or SEP.
This period allows for Medicare enrollment without penalty within eight months of losing employer coverage.
Understanding and utilizing the SEP can prevent unnecessary penalties.
4. Inadequate Coordination with Existing Coverage
A common mistake is not knowing if you need to enroll in Medicare Parts A and B, and failing to understand how Medicare coordinates with existing health insurance, particularly for those working beyond 65.
It’s crucial to determine whether Medicare will be your primary or secondary insurance.
This knowledge is vital to avoid overpaying for coverage and to ensure that healthcare needs are adequately met.




