What are the potential productivity impacts of new medications that treat Medicare beneficiaries?
One key aspect of many medications is that they not only help people feel better, but often these medications can help them re-enter the workforce, work more hours, work more productively, or all of the above. However, when evaluating new treatments for diseases that impact older Medicare beneficiaries (≥65 years), should we take into account productivity impacts?
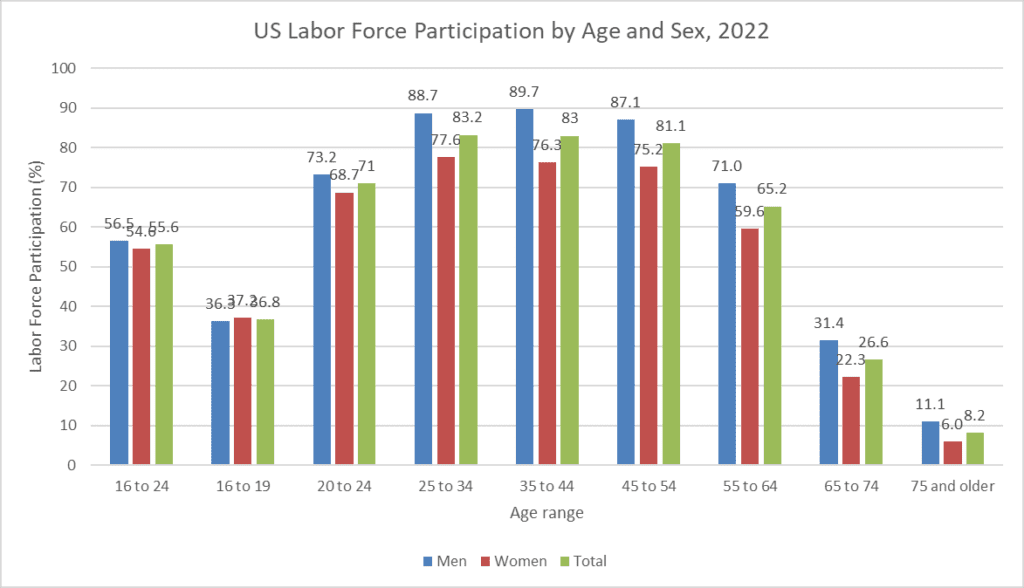
The first question to ask is, what share of individuals aged ≥65 years are actually in the labor force. Data form the Bureau of Labor Statistics (BLS) finds that 26.6% of individuals age 65-74 and 8.2% of individuals
≥75 years are in the labor force. Data from the Medicare Current Beneficiary Survey (MCBS) finds that “7.5 percent of beneficiaries were enrolled in Part A only, which includes people 65 and over who are still employed and may be covered by employer sponsored insurance (ESI).”
https://www.bls.gov/emp/tables/civilian-labor-force-participation-rate.htm
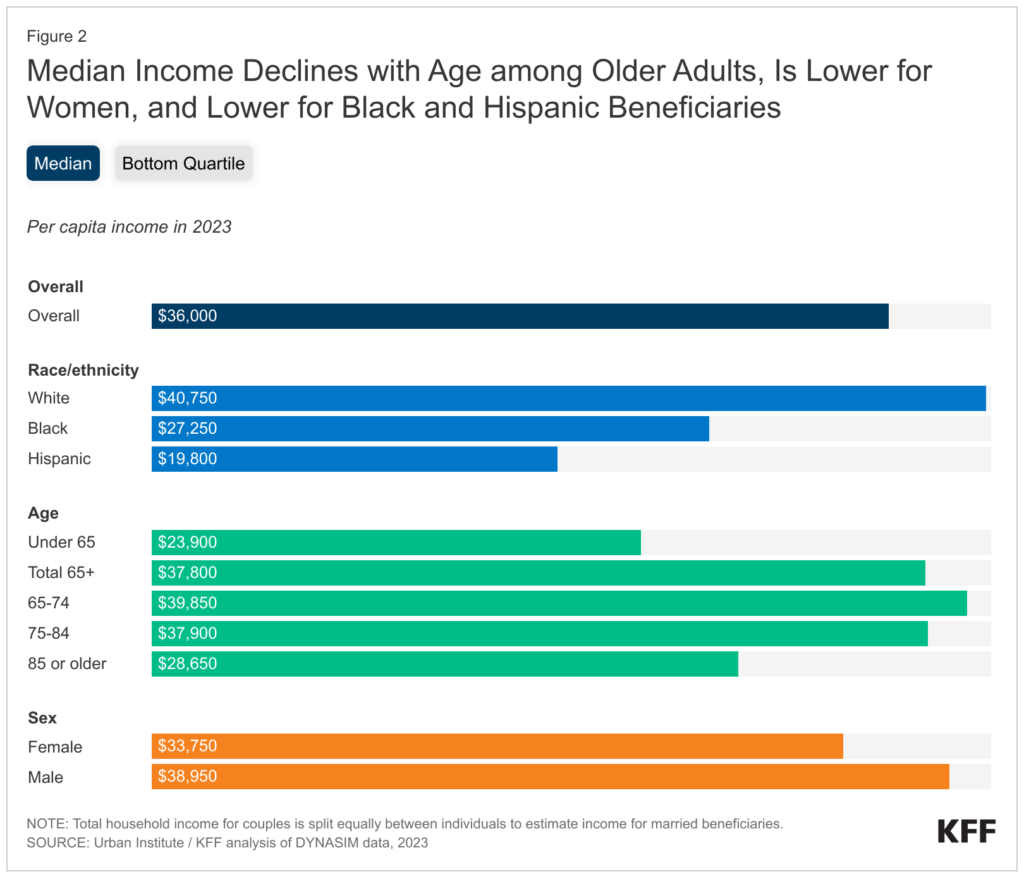
Medicare beneficiaries also earn significant income. The median income for Medicare beneficiaries is $36,000 overall and $37,800 or Medicare beneficiaries aged ≥65 years. These figures, however, include income from all sources (e.g., investments, Social Security) in addition to wage income.
 https://www.kff.org/medicare/issue-brief/income-and-assets-of-medicare-beneficiaries-in-2023/
https://www.kff.org/medicare/issue-brief/income-and-assets-of-medicare-beneficiaries-in-2023/
Many studies do not consider the impact of new medicines on non-market labor such as volunteering. However, a study by Grinshteyn and Sugar (2021) uses 2008-2018 Health and Retirement Study (HRS) data found that among older Americans 33.2% had volunteered in the past year.
In short, while the productivity impacts for older individuals are likely less then for working age individuals, they should not be ignored entirely.




