VERIFY: How to get your at-home COVID test reimbursed by health insurance – WUSA9.com
Find out who is an in-network provider of at-home COVID tests under your insurance plan before checking out. This will save you from filing for reimbursement later.
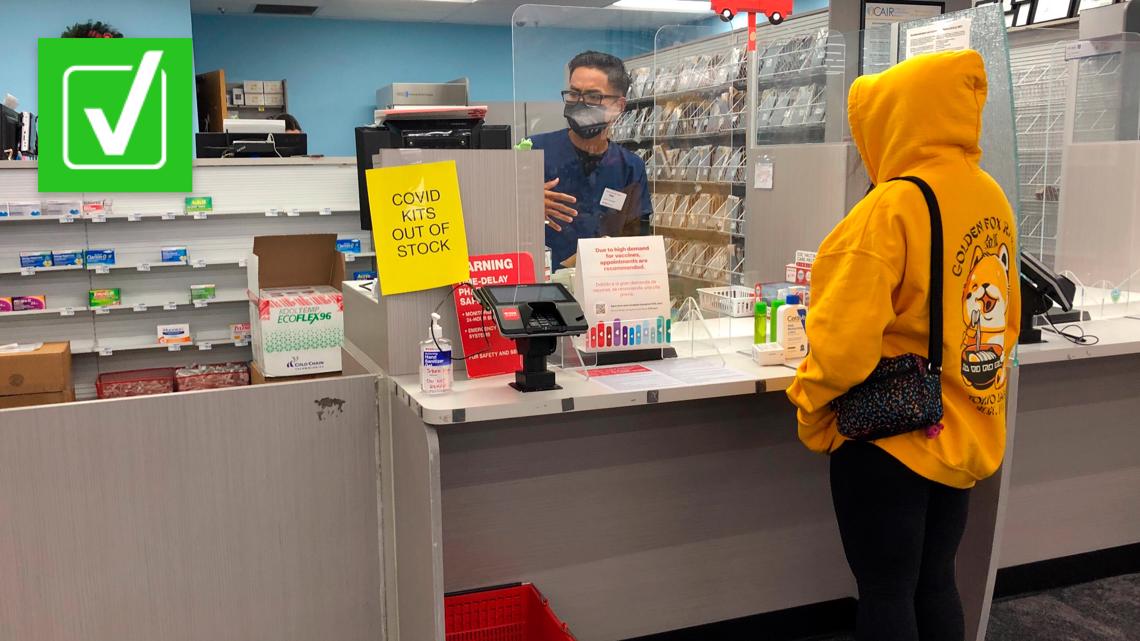
WASHINGTON — Millions of Americans can now pick up an at-home test kit from brick and mortar and online stores for free. That’s because the White House is making health insurance companies foot the bill.
President Biden announced the benefit back in early December. On Jan. 15, that benefit kicked in.
“The new coverage requirement means that most consumers with private health coverage can go online or to a pharmacy or store, buy a test, and either get it paid for up front by their health plan, or get reimbursed for the cost by submitting a claim to their plan,” the Department of Health and Human Services said recently. “This requirement incentivizes insurers to cover these costs up front and ensures individuals do not need an order from their health care provider to access these tests for free.”
So how exactly does it work?
THE QUESTION:
Do private health insurance companies now need to cover the cost of at-home COVID-19 test kits for customers?
THE SOURCES:
THE ANSWER:
Yes. Tests will be paid for in full if you go to an approved provider. Each insurance company may put out a list of different sellers in their network.
WHAT WE FOUND:
Private health insurers are now required to cover up to eight FDA-authorized at-home COVID tests per month for people on their plans. HHS specifies that you can get more kits covered by your insurance if your doctor deems the kits necessary.
“There is no limit on the number of tests, including at-home tests, that are covered if ordered or administered by a health care provider following an individualized clinical assessment, including for those who may need them due to underlying medical conditions,” HHS said.
How it works comes down to whether your insurance provider created a network of test providers. Think of it as “in-network” and “out-of-network” providers.
If your insurer has set up a network of preferred providers, including pharmacies, retailers and online vendors, you can go to any of those, show your insurance card, and walk out with your test. There’s no out-of-pocket expense and no forms to submit.
It’s less hassle for consumers, and it also may be cheaper for insurance companies.
If an insurer has a network in place, they can limit the per test reimbursement amount for retailers outside their network at $12 (or the price of the kit if cheaper), according to the Centers for Medicare and Medicaid Services.
Consumers are still allowed to buy kits out of network but you’ll only be reimbursed for up to $12 per individual test, according to CMS.
You’ll likely need to file some forms and go through the whole reimbursement process, so keep those receipts.
https://www.youtube.com/watch?v=-cUj4ZUAcR0
RELATED: Your COVID-19 antigen test result shows a faint line. Here’s what it could mean
If your insurance provider has not set up a list of providers by the time you purchase your kits, they’ve lost the ability to cap the cost at $12 and must pay you back the total cost of the kit, CMS said.
So, for example, if you buy a two-pack of tests for $34, the plan or insurer would have to reimburse you for that $34.
So yes, most insured Americans can now get at-home COVID test kits for free through their health insurance.
If you are uninsured, starting Jan. 19 the federal government will launch its Covidtests.gov website, where you can enter your address to order an at-home test kit directly to your doorstep. As of now, they say they will send out a maximum of four tests per household.
This is something journalists had previously pressed White House officials on.
For instance, in the days following the President’s announcements about insurance reimbursement, a reporter asked Press Secretary Psaki why kits weren’t being sent directly to people’s homes, similar what some European countries are doing.
One of these exchanges with Psaki went viral.
“Should we just send one to every American?”
Well, yeah. That’s not a bad idea.
pic.twitter.com/tdmrkB8uSQ
— Brian Robinson, Ph.D (@MrBrianRobinson) December 7, 2021
“That’s kind of complicated though. Why not just make them free and give them out to — and have them available everywhere?” a reporter asked.
“Should we just send one to every American?” Press Secretary Psaki responded.
Americans can order these at-home kits regardless of whether or not they have health insurance.
Some community health centers are also giving away tests for those without health insurance.
RELATED: How to get a COVID test without standing in the long lines
RELATED: Should you swab your throat to test for COVID? Experts are split




