Received letter asking for more information about treatment I received to see if someone other than Medicaid is responsible for the cost?
I am currently on Ohio Medicaid.
The questions are regarding whether or not I was in an accident or if the injury was the result of someone else’s actions. The treatment of I remember correctly was just a bunch of tests, blood work and urinalysis, after I complained of repeated symptoms. I had already been tested for for done of these things but I basically was persistent that there was something wrong so the retested me and added many other tests to that work up.
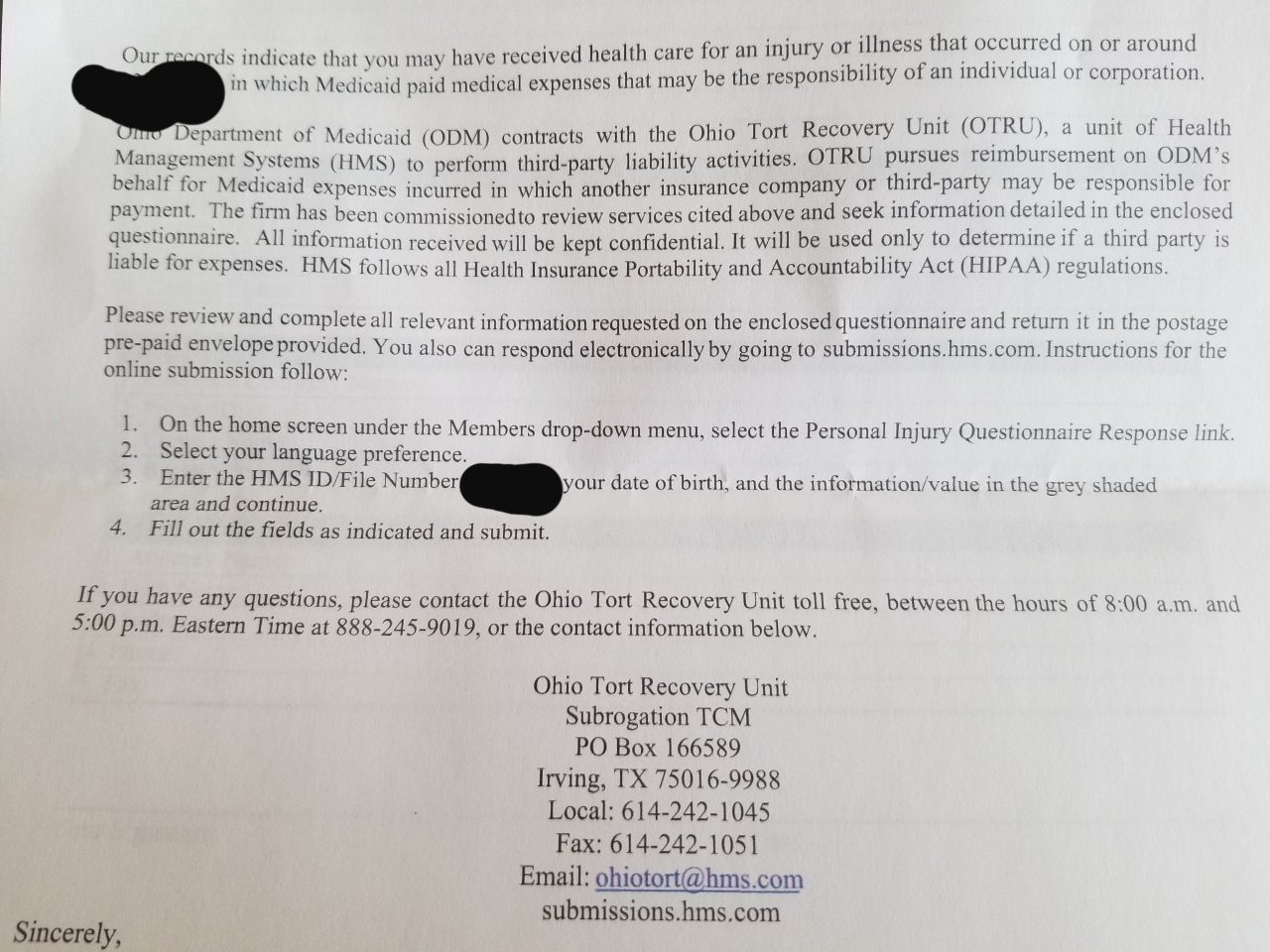
Just wondering if they’re trying to stick me with the bill. Either way I’m sure I have to respond, but I’m not sure if I should call and try to dispute or anything else.
Also, worth noting that I was in an accident a couple months AFTER the date listed for this treatment. I did go to the hospital to have some scans done that time, I don’t remember if they billed my insurance or how that worked at that time. Do you think they may have mistaked the tests and blood work I received for the scans and what not I had done following the accident? Including links for photos of the letter and questions for reference.
Sorry for the long, wordy be post. Thanks for any insight, much appreciated!






