Opinion: Address lack of mental health parity, don't make things worse! – The Connecticut Mirror
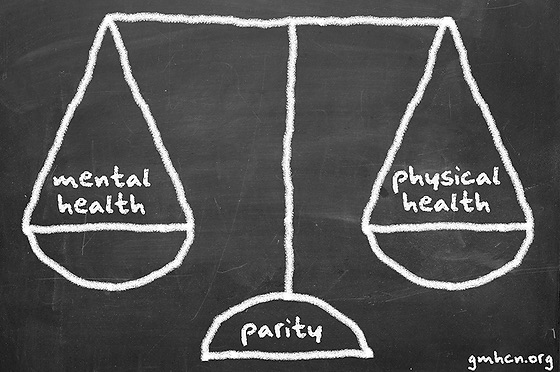
Everyone acknowledges the mental health crisis resulting from the COVID-19 pandemic. Addressing the mental health needs of Connecticut residents, particularly children, is a top priority this legislative session. Therefore, one has to question why a proposal that could potentially result in rolling back some of the progress we have made towards parity in access to mental health treatment remains under consideration.
HB 5042, An Act Concerning Healthcare Cost Growth, would grant authority to the Office of Health Strategy (OHS) to, among other things, set an annual healthcare cost growth benchmark and a primary care spending target. A proposal that would limit overall health care spending while increasing spending on primary care necessarily means that less money will be available for specialist care, including behavioral health care. Such a strategy will be detrimental to our efforts to achieve mental health parity.
First, the history. People living with mental health conditions or substance use disorders have been fighting for decades for parity in access to treatment. Advocates demanded parity laws because insurance companies did not provide coverage for mental health and substance use disorder treatment that was equal to the benefits provided for medical/surgical treatment of physical health issues. The first mental health parity law was passed at the federal level in 1996.
The Mental Health Parity Act (MHPA) provided that large group health plans could not cap mental health benefits at levels less than those imposed on medical/surgical benefits. Congress passed The Mental Health Parity and Addiction Equity Act (MHPAEA) in 2008 to impose similar restrictions on group health plans and health insurance issuers that provide mental health or substance use disorder (MH/SUD). The protections in the 2008 law were extended to apply to individual health insurance coverage under the Affordable Care Act (ACA) in 2010.
Connecticut enacted its first mental health parity law in 2000. That law required all individual and group health insurance plans that include coverage for physical health conditions to provide mental health coverage in their policies. In 2019, the Connecticut legislature unanimously passed, and Governor Lamont signed, Public Act 19-159, An Act Concerning Mental Health and Substance Use Disorder Benefits. This law required annual reports from insurance companies about their compliance with mental health parity laws, and the Insurance and Real Estate Committee to conduct an annual public hearing concerning such reports.
This session, the Insurance and Real Estate Committee has advanced another parity bill, SB 414, out of committee. This bill would require the Insurance Commissioner to report on the effectiveness of the mental health parity provisions in Connecticut law.
Currently the compliance certifications provided by individual companies on the Insurance Department website are out of date; the certifications are dated 2017, despite the fact that it is now 2022. Notably, in 2021, after an Insurance Department market conduct examination, companies that had self-certified in 2017 as compliant with mental health parity laws were found to be in violation.
The Insurance Department distributed funds from a Stipulation and Consent Order between United Healthcare Insurance Company, United Behavioral Health (collectively “UHC”) and its subsidiary Oxford Health Insurance, Inc. (Oxford), and the Insurance Department concerning UHC/Oxford’s violative practices related to behavioral health care services, to twenty behavioral health service-related agencies across Connecticut.
Recently, the Ninth Circuit Court of Appeals dealt a blow to mental health parity efforts in its ruling overturning the trial court decision in Wit v. United Behavioral Health. The trial court had ruled that the insurance company had violated its fiduciary duty to its customers seeking coverage for mental health and substance use disorders because it made its decisions to deny coverage according to its own guidelines and influenced by the company’s financial interests, rather than according to the accepted standards in the industry.
People already face barriers to care because of the lack of providers in the behavioral healthcare workforce. Existing parity laws may not be sufficient to ensure that insurance companies provide equivalent coverage for mental health conditions and substance use disorders, but at least there is a recognition of the need to address this. So why would we go backward? Passing a law that would grant authority to OHS to limit overall health care spending while directing more spending on primary care means less money available for specialist behavioral health care— it’s simple math. Our state’s lawmakers have chosen to recognize the severity of our mental health crisis. But at a time when people need greater access to behavioral health services, not less, this bill will place more obstacles in the way of people seeking care for mental health and substance use disorders.
Jordan Fairchild is the coordinator and community organizer for Keep The Promise Coalition. Kathy Flaherty is the executive director of Connecticut Legal Rights Project.




