New Nationwide Data on Outpatient Facility Fee Reforms
As hospitals and health systems expand their ownership and control of ambulatory care practices and physician offices, they frequently charge new facility fees for routine medical services delivered in outpatient settings. These additional bills drive up premiums and health expenditures for consumers, employers, and, ultimately, taxpayers. Consumers also face growing financial exposure to these facility charges as insurance deductibles increase and payers apply benefit designs that increase patients’ exposure to out-of-pocket costs, particularly in hospital outpatient settings. With support from and working in partnership with West Health, experts at Georgetown University’s Center on Health Insurance Reforms (CHIR) have identified and classified state laws regulating outpatient facility fee billing nationwide and have just released our findings in a set of maps available here.
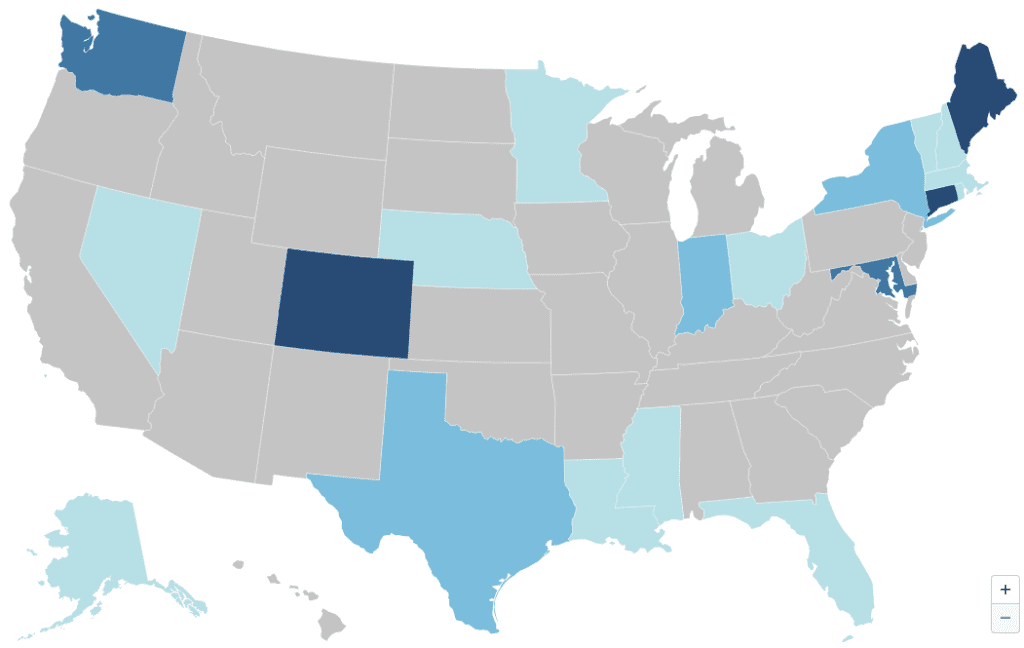
Twenty States Have Adopted At Least One Reform Strategy as of July 1, 2024
Twenty states, stretching across the country and representing a diversity of political orientations, have adopted at least one reform strategy as of July 1, 2024. These reforms include:
While their choice of tool varies, the broad array of states taking action is consistent with survey data showing widespread, bipartisan support for outpatient facility fee regulation.
Connecticut, Colorado, Maine, and Indiana Remain at the Forefront of Reforms
CHIR and West Health previously dug into how 11 study states have been approaching outpatient facility fee reforms. That effort identified Connecticut, Colorado, Maine, and Indiana as states at the forefront of regulation outpatient facility fee billing. Our new nationwide analysis confirms that these states have enacted the most comprehensive reforms to date.
Connecticut, Maine, and Indiana each have prohibited outpatient facility fee billing for routine medical services in certain hospital-owned settings. Colorado was the first state in the nation to require commercial claims forms to specify the actual office where care was delivered, with Maine, among other states, following in its footsteps more recently. All four states have also enacted between one and three other types of reforms, including public reporting or study requirements in all four states, consumer notification requirements in three, and out-of-pocket cost protections in two.
Incrementalism Is the Name of the Game
As the collection of laws in the above flagship states demonstrate, the various strategies for reforming outpatient facility fee billing are not mutually exclusive. But states typically tackle reform in an incremental fashion. The new maps reveal that most states have enacted only one type of reform for outpatient facility fee billing and most of these efforts are relatively modest: consumer notification requirements, study or reporting requirements, or prohibitions on facility fees limited to telehealth services. And no state in the nation has adopted site-neutral reforms in the commercial health insurance market, which would address the underlying incentives driving the growth of facility fees.
Nonetheless Connecticut—where lawmakers have gradually expanded their reforms over the past decade, including in the most recent legislative session—demonstrates that incremental steps can transform a state into a national leader.
Momentum Is Building, Despite Robust Industry Opposition
A few states, like Connecticut, Maine, and New Hampshire, began addressing this issue ten or more years ago, but most states with facility fee laws in effect enacted or amended their laws since 2021. Indeed, seven states passed facility fee reform legislation in the past 18 months alone. And more action appears on the horizon after an active 2024 legislative session, with several states launching task forces to study facility fees and potential reforms.
As happened with surprise billing reforms, state activity may well pave the way for federal reforms. Even in today’s polarized political atmosphere, there is bipartisan interest in Congress to enact “honest billing” requirements, facility fee prohibitions, and site-neutral payment reforms. These efforts are strongly supported by a wide variety of stakeholder groups itching for action. CHIR will continue to monitor and periodically update our maps to reflect ongoing developments in this area. Policymakers and advocates considering facility fee reforms are encouraged to contact CHIR experts for technical assistance at FacilityFeeTA@georgetown.edu.




