$15/no-deductible, Insurance said won’t cover. Why?
State: North Carolina
Medical Insurance: Anthem PPO
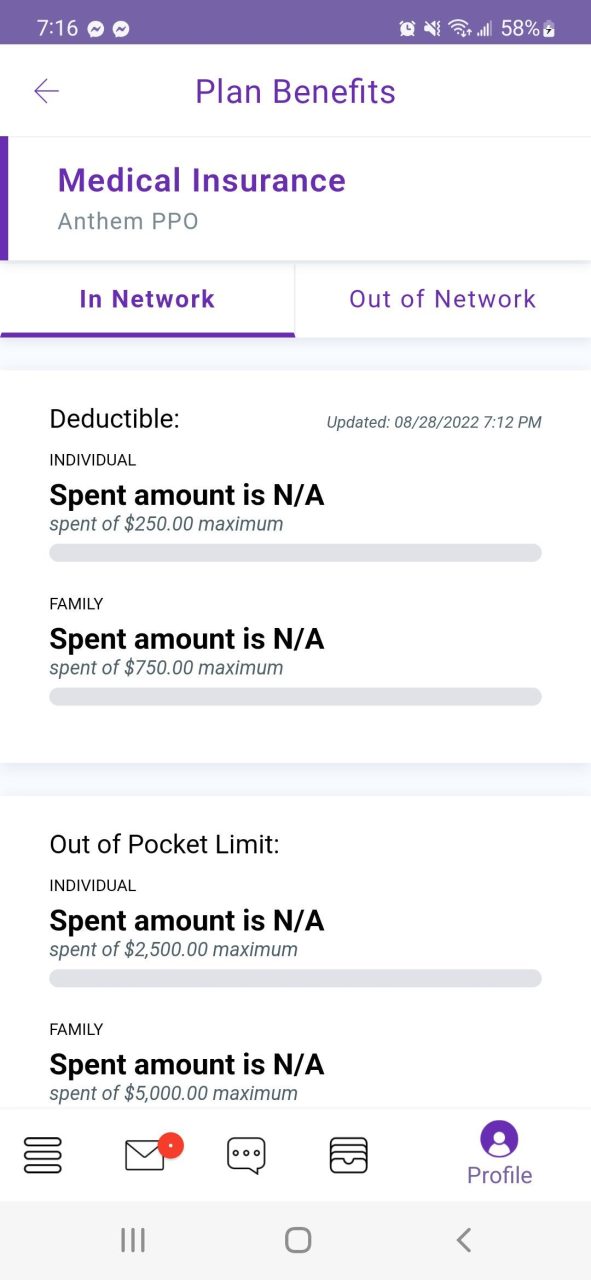
I’m very new to how health insurance works here in the US and it’s my first time, I thought I’m not going to have to pay for anything because it stated I have no deductible, the Health Insurance plan is shown in the picture.
Insurance plan – https://imgur.com/a/CgFdwhD
Two cases:
I had a dermatologist visit for a general check-up this year, code encoding they said which was double-checked was shoulder pain (I don’t even know why). Now Insurance didn’t pay anything at all even though they said the specialized visit is only $15/no-deductible on my plan. Now they said it’s on the not-covered part but I don’t see derma/skin related on the non-covered part in anthem.com or my plan. I had healthJoy(my company’s health app) verify it and they said the final resolution is I have to pay for it because the medical encoding (shoulder pain) does not fall on the insurance.
Had my first hearing general check-up, and the total cost was $422, they only paid $280, and I’m left with the rest. I thought this also falls in $15/no-deductible.
In the future, should I just ask first the front desk in the clinic if my insurance will cover anything? This makes me not want to get a check-up anymore and have a surprise bill.




