What are the new CMS Star Ratings Measures for 2025?
My FTI colleagues Mark Van Ert and Krunal Patel summarize some of the new quality measures that will be incorporated into the 2025 CMS Star Ratings that are used to evaluate Medicare Advantage (MA) plans. The CMS Star Ratings are very important as CMS payments to MA plans is expected to increase by 3.7% or $16 billion between 2024 and 2025.
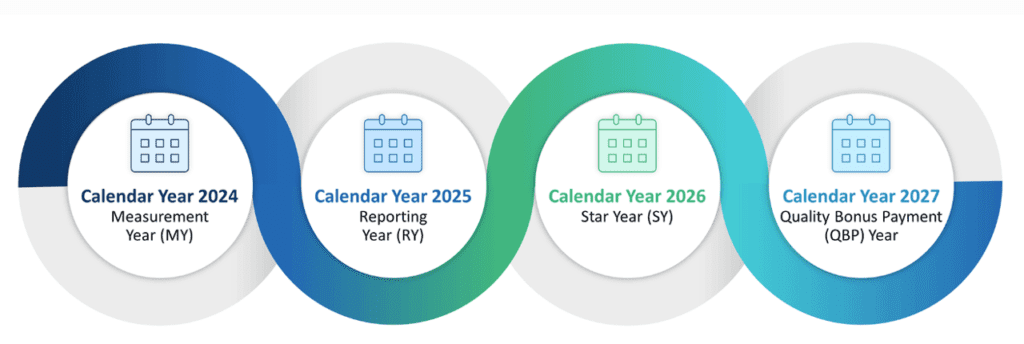
Van Ert and Patel describe the CMS ratings cycle as follows:
Star ratings are determined through a four-year process. The first year is the measurement year (“MY”), in which plans collect performance data for various measures, though specific timing can vary — for instance, Consumer Assessment of Healthcare Providers and Systems (“CAHPS”) surveys are conducted at the start of the second year. During the second year — the reporting year (“RY”) — the CMS evaluates the previous year’s performance data. The third year is the Star Year (“SY”), which is when the Star Ratings are officially assigned. In the fourth year — the quality bonus payment (“QBP”) year.4
https://www.fticonsulting.com/insights/articles/cracking-code-2025-cms-star-ratings
Which are the new measures to be included for 2025? These include:
Concurrent Use of Opioids and Benzodiazepines. Evaluates the simultaneous prescription of opioids and benzodiazepines, which significantly increases the risk of respiratory depression and fatal overdoses Use of Multiple Anticholinergic Medications in Older Adults. Measure focuses on the risks associated with older adults taking multiple anticholinergic medications concurrently, which can lead to cognitive decline.Kidney Health for Patients with Diabetes. Measures the percentage of members aged 18-85 with diabetes (type 1 and type 2) who received a kidney health evaluation, which includes evaluations of estimated glomerular filtration rate (eGFR) and a urine albumin-creatinine ratio (uACR). Improving/Maintaining Physical Health. Measures overall physical functioning based on the Medicare Health Outcomes Survey. Improving/Maintaining Mental Health. Evaluates self-reported beneficiary data regarding emotional well-being, such as the frequency of feelings of depression, anxiety and other mental health conditions based on the Medicare Health Outcomes Survey.
Full technical specifications of all CMS Star Rating quality measures can be found here.





