Out of network anesthesia – NSA question
I got a strange letter/quasi bill in the mail today that is leaving me confused and thinking something less than reputable is going on.
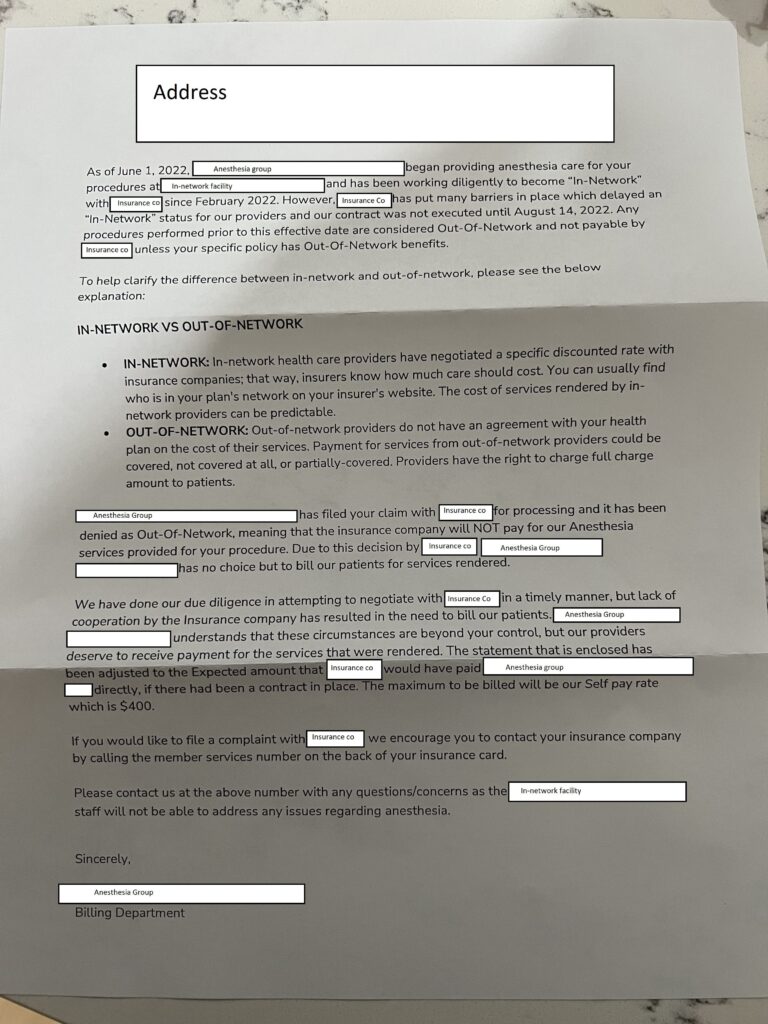
Background: I had a procedure last year (June 2022) at an in-network facility. It involved anesthesia. A non-emergency procedure, but 100% in-network facility and no notice was ever given of anything not being in-network (that I recall, it was 8 months ago now…). Skip forward to today, and I get this letter:
My two questions I guess are as follows:
First: I was under the impression the no surprises act blocked bills like this. An out of network charge at an in network facility then being billed directly to me as a patient? The letter states they’re charging me “what my insurance would have paid” as if it’s a favor, but I thought I couldn’t be charged anything other than what my copay would have been with my insurance?
Second: The letter says they “deserve” to be paid, not that I “owe” the balance. Is this some sneaky method to try to trick people into paying something they don’t owe? It seems really suspect how they worded it.
Obviously I’m going to call my insurance company and the originator of this letter (a “consultant group”?), but I was hoping to be armed with some knowledge beforehand, if anyone here has experience or input on something like this. It just seems like this company/group decided to go ahead and start offering services before they got a contract worked out, and is now trying to shift their mistake onto unsuspecting patients.