Medicaid Program Managers Will Be Robocalling
What You Need to Know
Rule changes could cause 16 million Medicaid enrollees to lose their coverage starting this spring.
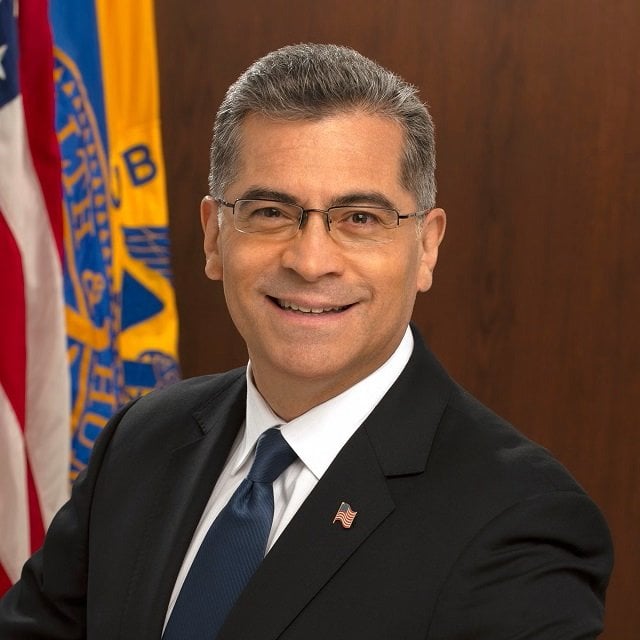
HHS Secretary Xavier Becerra asked for permission for Medicaid program vendors to use automated systems to warn the enrollees.
Supporters told the FCC that robocalling is a great way to keep Medicaid enrollees covered.
The Federal Communications Commission has given the Medicaid program — including state program managers, Medicaid managed care plan providers and program marketing vendors — permission to use automated communications systems to warn enrollees about changes in coverage rules.
FCC says the U.S. Department of Health and Human Services, the department that oversees Medicaid, and other organizations that help run Medicaid to robocall and robotext each enrollee about six to eight times.
FCC approved the Medicaid robocalling and robotexting campaign in response to a request sent by HHS Secretary Xavier Becerra and provided a testimonial to the potential effectiveness of telemarketing campaigns.
Many commenters wrote to tell the FCC that millions of the 98 million people now enrolled in Medicaid are on track to lose their coverage because of an end to temporary provisions put in place to help get the enrollees through the COVID-19 pandemic.
“These commenters indicate that the use of autodialed calls and text messages are highly effective in reaching the most vulnerable groups such as low-income, elderly and non-English speaking individuals with the information that they require to maintain these health care benefits,” Alejandro Roark, chief of the FCC’s Consumer and Governmental Affairs Bureau, wrote in a ruling approving Becerra’s request.
The Basics
Medicaid is a program funded and run partly by state government agencies and partly by HHS that provides health coverage for low-income Americans and many low-income and middle-income people who qualify for nursing-home-level care.
The program and a related program for children were providing coverage for about 73 million people in 2019, before the pandemic started.
Congress then halted eligibility Medicaid redeterminations, or efforts to detect and eject enrollees who no longer qualify for Medicaid, in an effort to maximize the number of Americans with some kind of health coverage.




