What is the impact of delayed lung cancer diagnosis on outcomes?
One would think that this question would be a relatively
easy question to answer empirically: simply compare patients with delays
against those without delays and see if there is a difference in health
outcomes (e.g., survival). This
approach, however, is problematic as due to three key methodological concerns.
Measurement issues. Ideally, one would like to compare patients
at a given stage who are diagnosed and treated for lung cancer against those
who are not. However, the underlying lung
cancer stage is typically unobserved during portions of the delay in care either
because a lung cancer diagnosis is not made yet or perhaps it is made but full
staging has not yet been completed. Mediators. A mediator is a variable lies
in the causal path between the exposure variable and the outcome of interest. For instance, consider two patients (Patient
A and B) with stage III lung cancer, but this stage information is not yet known
to the researcher. Consider the case where
Patient B’s tumor advances to stage IV during the diagnostic phase whereas
Patient A’s tumor remains at Stage III. In
this case, it appears to the researcher that Patient A is a Stage III patient
and Patient B is a Stage IV patient.
Here the worsening outcome (stage progression) leads to stage
advancement. The problem is that the
researcher may compare Patient B with other Stage IV patients without a delay
and Patient B may have better outcomes than those regular Stage IV patients
since Patient B’s tumor only just advanced. Confounders. Confounding occurs when a third variable
influences both the exposure and outcome variable. For instance, it could be the case that when interventional
pulmonologists view a lesion, they may view it as high or low risk. High risk patients may get diagnosed rapidly;
low risk patients may be more likely to have a diagnostic delay. When comparing outcomes, it would thus appear
that those with diagnostic delays had better outcomes. However, it is really a third variable (i.e.,
lesion risk) which is causing both the delay period and outcomes.
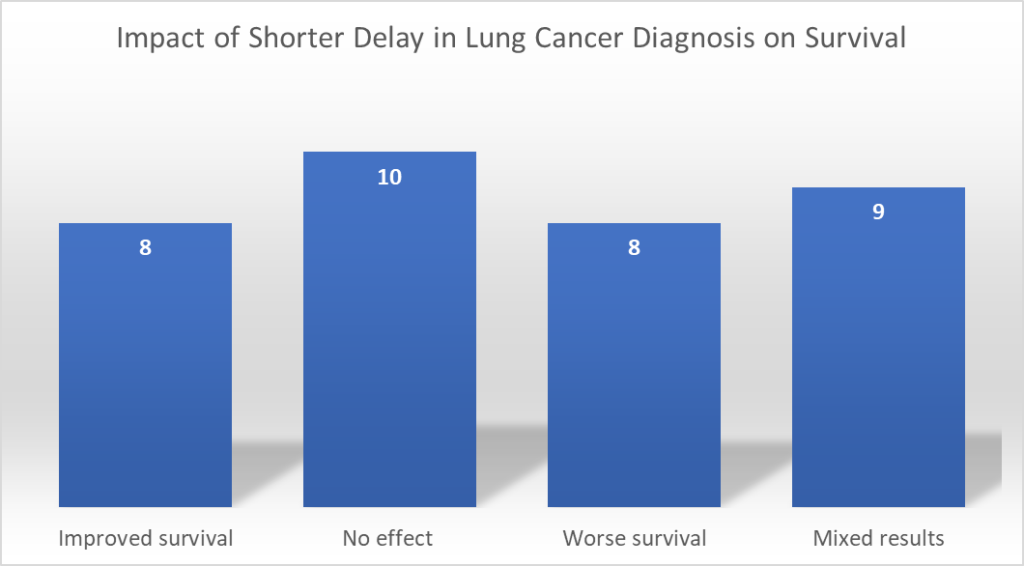
In part because of these methodological complexities, a systematic literature review by Zuniga and Ost (2021) finds some counterintuitive results. They find that longer delays lead to worse survival for n=8 studies, no statistically significant effect of delay on survival for n=10 studies, and a paradoxical effect that longer delays lead to better survival for n=8 articles, and mixed results (some strata worse and others paradoxical or no effect) for n=9. The degree to which we observe so many counterintuitive impacts clearly suggests that mediators and confounding are significant empirical issues that have not been fully addressed across studies.
Below are the relevant articles. Articles in bold show shorter delay leads to better survival; italics show shorter delay lead have no effect; underlined means shorter delay leads to worse outcomes, and no formatting means that shorter delay leads to mixed survival outcomes depending on the group.
Kanashiki M, Satoh H, Ishikawa H, Yamashita YT, Ohtsuka M, Sekizawa K. Time from finding abnormality on mass-screening to final diagnosis of lung cancer. Oncol Rep. 2003;10(3):649-652.Kashiwabara K, Koshi S, Itonaga K, Nakahara O, Tanaka M, Toyonaga M. Outcome in patients with lung cancer found on lung cancer mass screening roentgenograms, but who did not subsequently consult a doctor. Lung Cancer. 2003;40(1):67-72. Buccheri G, Ferrigno D. Lung cancer: clinical presentation and specialist referral time. Eur Respir J. 2004;24(6):898-904. Kanarek NF, Hooker CM, Mathieu L, et al. Survival after community diagnosis of early-stage non-small cell lung cancer. Am J Med. 2014;127(5):443-449. Labbe C, Anderson M, Simard S, et al. Wait times for diagnosis and treatment of lung cancer: a single-centre experience. Curr Oncol. 2017;24(6):367-373. Yang CJ, Wang H, Kumar A, et al. Impact of timing of lobectomy on survival for clinical stage IA lung squamous cell carcinoma. Chest. 2017;152(6):1239-1250. Khorana AA, Tullio K, Elson P, et al. Time to initial cancer treatment in the United States and association with survival over time: an observational study. PLoS One. 2019;14(3):e0213209. Cushman TR, Jones B, Akhavan D, et al. The effects of time to treatment initiation for patients with non-small-cell lung cancer in the United States. Clin Lung Cancer. 2021;22(1):e84-e97. Ringbaek T, Borgeskov S, Lange P, Viskum K. Diagnostic and therapeutic process and prognosis in suspected lung cancer. Scand Cardiovasc J. 1999;33(6):337-343. Aragoneses FG, Moreno N, Leon P, et al. Influence of delays on survival in the surgical treatment of bronchogenic carcinoma. Lung Cancer. 2002;36(1):59-63. Kashiwabara K, Koshi S, Ota K, Tanaka M, Toyonaga M. Outcome in patients with lung cancer found retrospectively to have had evidence of disease on past lung cancer mass screening roentgenograms. Lung Cancer. 2002;35(3):237-241. Pita-Fernandez S, Montero-Martinez C, Pertega-Diaz S, Verea- Hernando H. Relationship between delayed diagnosis and the degree of invasion and survival in lung cancer. J Clin Epidemiol. 2003;56(9): 820-825. Berthelet E, Truong PT, Lesperance M, et al. Examining time intervals between diagnosis and treatment in the management of patients with limited stage small cell lung cancer. Am J Clin Oncol. 2006;29(1):21-26. Liberman M, Liberman D, Sampalis JS, Mulder DS. Delays to surgery in non-small-cell lung cancer. Can J Surg. 2006;49(1):31-36. Loh LC, Chan LY, Tan RY, et al. Time delay and its effect on survival in malaysian patients with non-small cell lung carcinoma. Malays J Med Sci. 2006;13(1):37-42. Bryant AS, Cerfolio RJ. Differences in outcomes between younger and older patients with non-small cell lung cancer. Ann Thorac Surg. 2008;85(5):1735-1739. Shin DW, Cho J, Kim SY, et al. Delay to curative surgery greater than 12 weeks is associated with increased mortality in patients with colorectal and breast cancer but not lung or thyroid cancer. Ann Surg Oncol. 2013;20(8):2468-2476. Malalasekera A, Blinman PL, Dhillon HM, et al. Times to diagnosis and treatment of lung cancer in New South Wales, Australia: a multicenter, Medicare data linkage study. J Oncol Pract. 2018;14(10): e621-e630. Myrdal G, Lambe M, Hillerdal G, Lamberg K, Agustsson T, Stahle E. Effect of delays on prognosis in patients with non-small cell lung cancer. Thorax. 2004;59(1):45-49. Comber H, Cronin DP, Deady S, Lorcain PO, Riordan P. Delays in treatment in the cancer services: impact on cancer stage and survival. Ir Med J. 2005;98(8):238-239. Salomaa ER, Sallinen S, Hiekkanen H, Liippo K. Delays in the diagnosis and treatment of lung cancer. Chest. 2005;128(4):2282-2288 Annakkaya AN, Arbak P, Balbay O, Bilgin C, Erbas M, Bulut I. Effect of symptom-to-treatment interval on prognosis in lung cancer. Tumori. 2007;93(1):61-67. Gould MK, Ghaus SJ, Olsson JK, Schultz EM. Timeliness of care in veterans with non-small cell lung cancer. Chest. 2008;133(5):1167-1173 Gonzalez-Barcala FJ, Falagan JA, Garcia-Prim JM, et al. Timeliness of care and prognosis in patients with lung cancer. Ir J Med Sci. 2014;183(3):383-390. Nadpara PA, Madhavan SS, Tworek C. Disparities in lung cancer care and outcomes among elderly in a medically underserved state population-a cancer registry-linked database study. Popul Health Manag. 2016;19(2):109-119. Abrao FC, de Abreu I, Rocha RO, Munhoz FD, Rodrigues JHG, Batista BN. Interaction between treatment delivery delay and stage on the mortality from non-small cell lung cancer. J Thorac Dis. 2018;10(5):2813-2819. Bozcuk H, Martin C. Does treatment delay affect survival in nonsmall cell lung cancer? A retrospective analysis from a single UK centre. Lung Cancer. 2001;34(2):243-252. Quarterman RL, McMillan A, Ratcliffe MB, Block MI. Effect of preoperative delay on prognosis for patients with early stage non-small cell lung cancer. J Thorac Cardiovasc Surg. 2003;125(1):108-113. Radzikowska E, Roszkowski-Sliz K, Chabowski M, Glaz P. Influence of delays in diagnosis and treatment on survival in small cell lung cancer patients. Adv Exp Med Biol. 2013;788:355-362. Gomez DR, Liao KP, Swisher SG, et al. Time to treatment as a quality metric in lung cancer: staging studies, time to treatment, and patient survival. Radiother Oncol. 2015;115(2):257-263. Nadpara P, Madhavan SS, Tworek C. Guideline-concordant timely lung cancer care and prognosis among elderly patients in the United States: a population-based study. Cancer Epidemiol. 2015;39(6):1136-1144 Kasymjanova G, Small D, Cohen V, et al. Lung cancer care trajectory at a Canadian centre: an evaluation of how wait times affect clinical outcomes. Curr Oncol. 2017;24(5):302-309. Vinod SK, Chandra A, Berthelsen A, Descallar J. Does timeliness of care in non-small cell lung cancer impact on survival? Lung Cancer. 2017;112:16-24. Alanen V, Koivunen JP. Association of diagnostic delays to survival in lung cancer: single center experience. Acta Oncol. 2019;58(7): 1056-1061. Tsai CH, Kung PT, Kuo WY, Tsai WC. Effect of time interval from diagnosis to treatment for non-small cell lung cancer on survival: a national cohort study in Taiwan. BMJ Open. 2020;10(4): e034351.